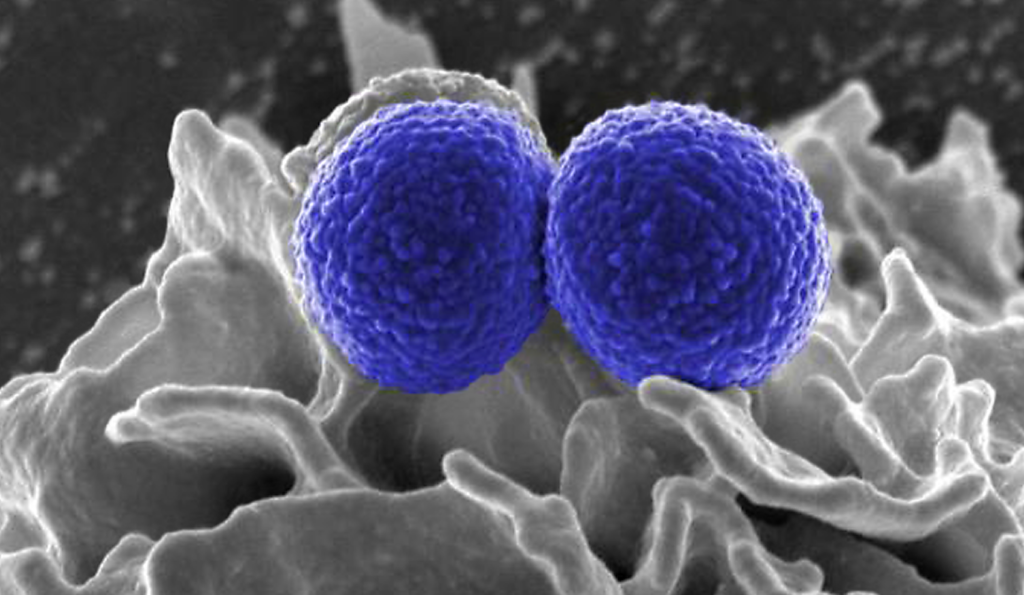
This digitally colorized, scanning electron microscopic (SEM) image, depicts two blue-colored, spherical, methicillin-resistant, Staphylococcus aureus (MRSA) bacteria, that were in the process of being phagocytized by an uncolored, human white blood cell (WBC). The bacteria shown are members of the strain MRSA252, a leading cause of hospital associated, nosocomial infections in the United States, and United Kingdom.
Image Credit: National Institute of Allergy and Infectious Diseases (NIAID)

Skin and soft tissue infections have become a steadfast issue faced in communities and healthcare facilities alike. While those that were found to be methicillin-resistant Staphylococcus aureus (MRSA) used to represent a novel threat in the antimicrobial resistance (AMR) battle, they are now so common that isolation precautions are often not used. The true burden of MRSA is exceedingly difficult to quantify, with some estimates of colonization in elderly care facilities noting a pooled prevalence of 14.69%, it has been widely accepted that roughly 30% of healthy people are colonized with S aureus.1 More and more though, global reports on AMR note that MRSA is exceedingly common and represents one of many resistant infections that is no long emerging but wholly endemic.
While MRSA infections can present in many different modalities, the presence of it in skin and soft tissue (SST) infections can pose a public health and infection prevention hazard. A new study published in Emerging Microbes & Infections, assessed the epidemiology and clinical features of MRSA TSS infections including virulence factors such as Panton-Valentine leucocidin (PVL)-positive and negative.2 As PVL positivity has implications for clinical and treatment outcomes, especially in deep abscesses and recurrent SST infections, understanding the epidemiology of PVL detection is of importance. As such, the researchers worked to understand the clinical characteristics of SST infections in those patients who experienced PVL-positive and PVL-negative MRSA infections. Assessing patients diagnosed with SST infections as a result of MRSA, within the First Affiliated Hospital of Zhejiang University School of Medicine from January 2014 to December 2020, they performed whole-genome sequencing and molecular analysis, in addition to medical record review.
What You Need to Know
Methicillin-resistant Staphylococcus aureus (MRSA) has become endemic in both community and healthcare settings.
The study highlighted that PVL-positive MRSA skin and soft tissue infections (SSTIs) are more frequently associated with abscess formation and typically require surgical drainage rather than antimicrobial treatment.
PVL-positive MRSA infections are more likely to be community-associated and are often found in specific hospital departments such as orthopedics and dermatology.
Analysis found that “PVL-positive patients had shorter hospital stays (mean, 9 vs. 24 days; p < 0.001) and abscess resolution durations (mean, 8 vs. 13 days; p < 0.01). PVL-positive MRSA-induced SSTIs were more frequently associated with abscesses [36/55 (65.5%) vs. 15/124 (12.1%), p < 0.001], with 52.7% undergoing incision and drainage; over 80% of PVL-negative patients received incision, drainage, and antibiotics. In PVL-positive patients receiving empirical antibiotics, anti-staphylococcal agents such as vancomycin and linezolid were administered less frequently (32.7%, 18/55) than in PVL-negative patients (74.2%, 92/124), indicating that patients with PVL-positive SSTIs are more likely to require surgical drainage rather than antimicrobial treatment.”
The most predominant lineage was ST59, with a total of 907 MRSA strains isolated, 21.7% of which had the PVL gene. From a community health perspective, it’s important to note that a larger proportion of PVL-positive MRSA infections were community-associated, and while cases were found across 8 hospital wards, most were found within orthopedics, hand surgery, and the dermatology departments. Moreover, those patients with PVL-negative MRSA had higher rates of having a diabetic foot and infected trauma wounds, as well as surgical site infections.
Lastly, the authors did note that in terms of MRSA susceptibility, all isolates were vulnerable to vancomycin, linezolid, nitrofurantoin, quinupristin/dalfopristin, tigecycline, and daptomycin. Such insights into MRSA SST infections are critical in understanding not only their clinical presentations and epidemiology, but the importance of postoperative education in MRSA colonization and infection prevention efforts.