Traditionally, dental patients undergoing surgical procedures have often been prescribed antibiotics for prophylaxis purposes. For example, in patients with heart issues there were concerns over bacterial endocarditis that prompted this practice, but newer studies around this topic have shifted the need for antibiotics. “Guidance by the National Institute for Health and Care Excellence (NICE) in England and Wales states that antibiotic prophylaxis against infective endocarditis is not recommended routinely for people undergoing dental procedures.”1
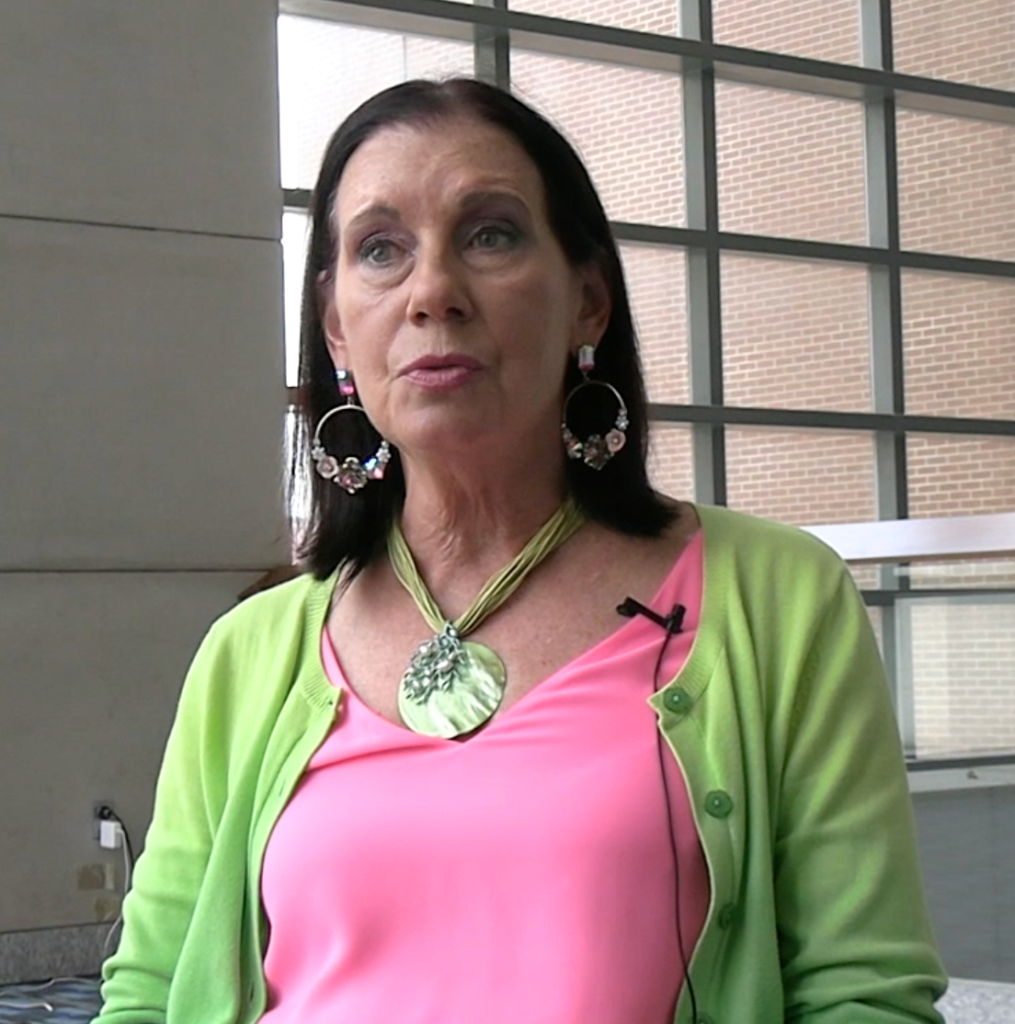
Debra Goff, PharmD, professor of Pharmacy Practice, The Ohio State University Wexner Medical Center, has been studying the subject of dentistry and antimicrobial stewardship for a number of years. She has become an advocate for the field and teaching dentists to understand fully the nuances of stewardship and how antimicrobial prescribing practices have changed.
“The CDC [Centers for Disease Control and Prevention] published a great study that said, ‘25 million prescriptions a year are prescribed by dentists.’ But, when I looked into the details of that, that only represents general dentists working in the VA health care system,” Goff said. “I’m working with private practice dentists, which represent 80% of dentists in the United States, and the specialists, the oral surgeons, the periodontists, and the endodontists who need antibiotics… they prescribe a phenomenal volume of antibiotics. Some of them are necessary, but a lot of them [are not]. And the durations they’re using are the old football scores—10 and 14 days, and they can do better. There’s no evidence to support those long durations.”
As part of Goff’s dental stewardship advocacy, she speaks to dentists offering guidance on prescribing practices for patients with penicillin allergies and some of the therapies that have been replaced as alternatives most especially as it relates to clindamycin, and concerns associated with contracting C difficile when taking the antibiotic.
“They use clindamycin routinely for pen allergic patients, because no one’s told them not to…There’s evidence to use different antibiotics for the pen allergic patient.”
Goff mentioned a dentist who herself contracted C diff after taking clindamycin for a dental procedure and the dentist credited the work of the C diff advocacy group Peggy Lillis C diff Foundation in helping her finding out about live biotherapeutic products for C diff, and was successfully treated with that modality.
Goff says for private practice dentists there is very little information coming to them due to the scope of their responsibilities. For example, dentists may still be prescribing longer durations for patients—the aforementioned 10-14 day paradigm—whereas, in the hospital settings, providers have decreased duration times greatly.
“We’re down to 3 and 5 days for some durations. So, I’ve really started challenging the dentists,” Goff said. “In private practice, they don’t do research. It’s not part of their practice, so there’s very little evidence. But they have been very engaged in understanding now they could be harming patients.”
Goff served on a panel at last week’s World AMR Congress and she sat down with Contagion to discuss stewardship in a few areas. In the first part of our 2-part interview with Goff, she discusses dental stewardship and bringing the message of the changing prescribing practices and dealing with penicillin allergies to this medical field.