HIV is longterm, progressive illness that progressively compromises the immune system, making the body vulnerable to a wide range of opportunistic infections and cancers. The extensive ramifications of the HIV/AIDS pandemic have left a lasting impression on various regions of the world, with Sub-Saharan Africa facing especially severe challenges.1
HIV prevalence varies significantly by region, highlighting the complexity of the epidemic. The Caribbean, for example, has become one of the most affected regions, emulating some parts of Africa.2
As the world struggles with the ongoing consequences of the HIV pandemic a thorough understanding of the various ways the virus spreads and its subtle effects on different populations is crucial. This understanding serves as the foundation for the creation and application of efficient prevention and treatment plans which in turn promotes an international endeavor to lessen the pervasive effects of AIDS on people and communities around the world.3
Case Presentation
A 50-year-old male patient was admitted to the medical unit with chief complaints of severe infection, vomiting, cough with sputum, and fever. On the first examination, physicians suggested it could be viral encephalitis or alternative diagnoses included endocarditis, pulmonary tuberculosis, hyponatremia and HIV. The patient was having a fungal susceptible growth on the face, which indicated it was a compromised immune system. As the patient had a critical condition it was hard to conquer a core diagnosis of the condition.
Later on, the patient was run over robust pathological examinations for a precise decision about the diagnosis. Suggested medical tests were blood culture test, HIV serology and sputum examination for the possible diagnosis. An initial prophylactic therapy was started including ceftriaxone and vancomycin each in 1g IV.
Final Diagnosis
After the availability of tests, the patient was diagnosed with HIV.
Epidemiological and Medical History
The patient had no chronic history of illness and allergy. He had started coughing a few weeks ago and experienced a few weak immune symptoms. He was using generic anti-allergic and paracetamol for cough and fever. Later, he had been prescribed Augmentin 675 mg (Amoxicillin and Clavulanic acid).
Prescribed Medications
On the eve of the emergency, the patient was started on ceftriaxone and vancomycin intravenously to cover the prophylactic coverage. After the sampling of patients, physicians prescribed antimicrobials listed in Table 1.
Interventions
As part of a team, we assessed the medication therapy of patients in that unit. For coverage, the prescriber had suggested many antibiotics to control the patient’s health. On more inquiry to the patient, it was revealed that he had been suffering from some adverse effects of therapy, ie, nephropathic manifestations including pain, diarrhea, intensity in fungal growth and low platelet count.
On further discussion with the prescriber, all these drugs were prophylactically given to the patient even though the patient had not started proper HIV treatment. The following interventions were proposed:
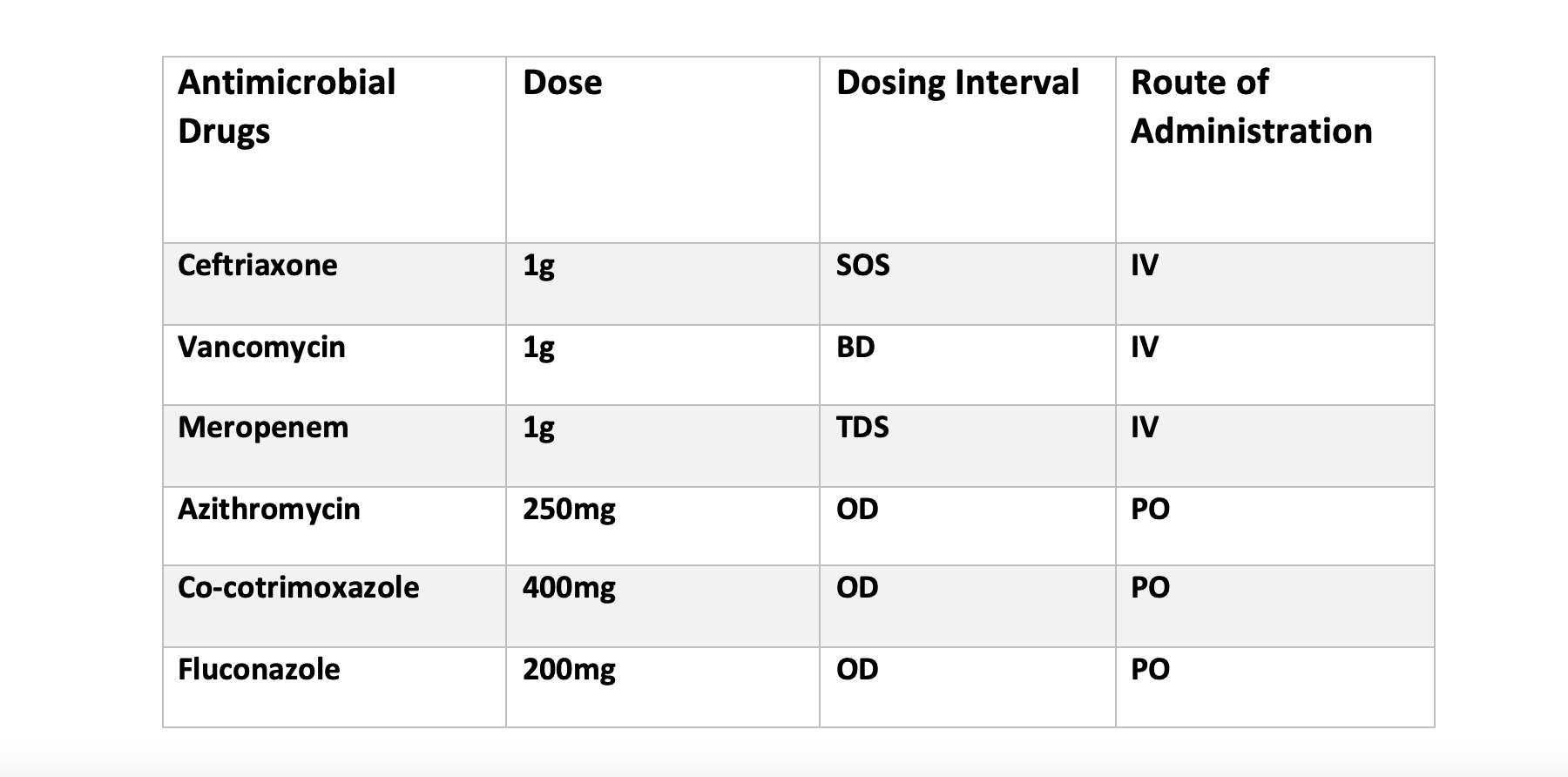
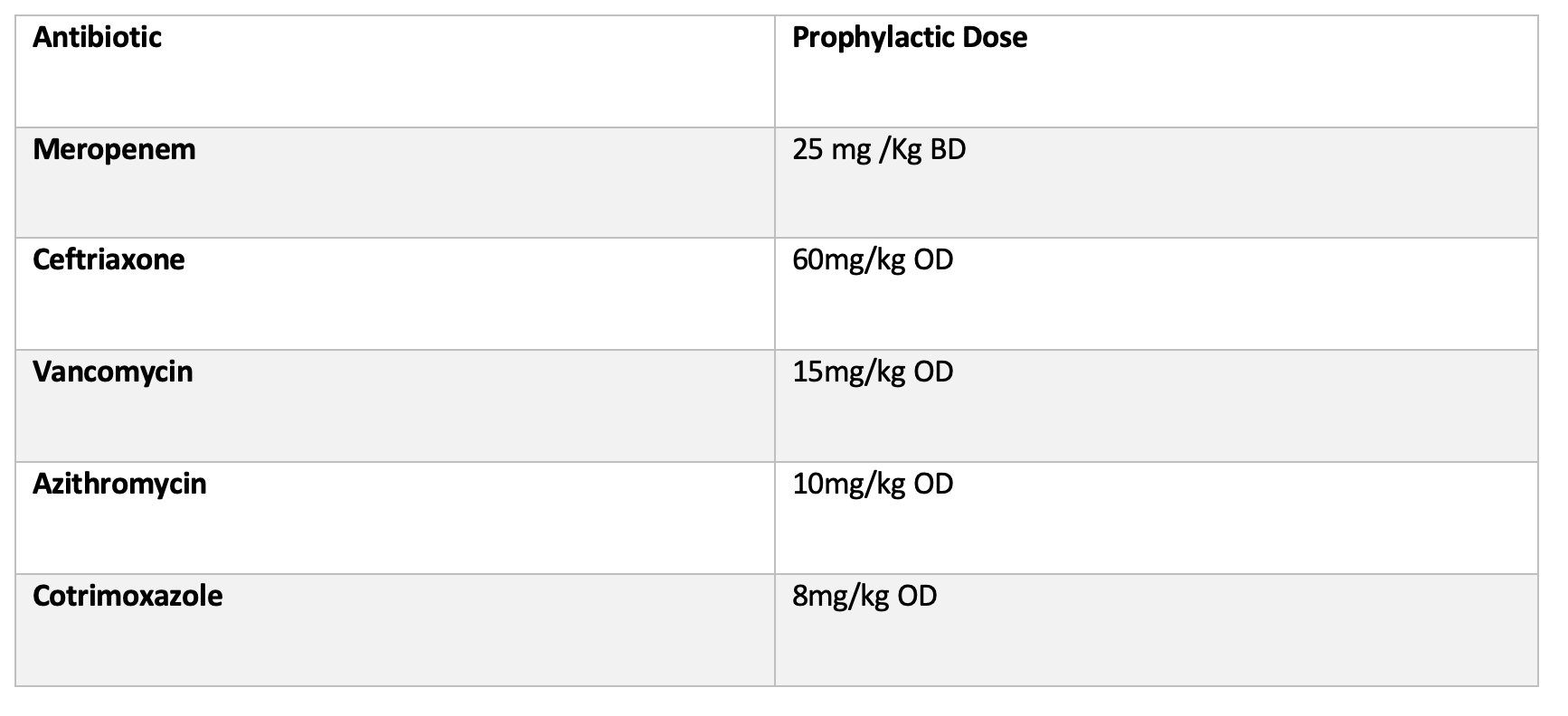
- De-escalation of all antimicrobials were proposed. Doses were reduced according the guidelines of ASHP for Prophylactic Doses which are labeled in Table 2.
- Three antibiotics with possible broad spectrum were given including ceftriaxone, vancomycin and meropenem. Only meropenem remained in therapy on prophylactic dose and the others were discontinued.
- A call from HIV consultancy clinic was addressed for targeting therapy because prescriber stated they could not use targeting therapy in general medical units.
- HIV antiviral therapy was addressed at proper doses to reduce the potential spread of HIV.
- Culture sensitivity reports and tests were recommended to prescribers.
Figure 2. Suggested Prophylactic doses for this patient for interventions.
Stewardship Protocols
All proposed interventions were according to the guidelines of Infectious Diseases Society of America and World Health Organization for antimicrobial stewardship (AMS).4
The form describes the following special documentation:
- Demographical data of patient
- Clinical data including Diagnosis details
- Microbiological data including serology details
- Antimicrobial Prescription including agents prescribed
- Initial review of the patient after 24 hrs
- Secondary review of patient after 48 hrs
- Prescribers and pharmacist’s comments
Treatment and Follow-Ups
As mentioned in stewardship protocols, two post interventional follow ups were conducted. One after 24 Hours and one after 48 Hours. Significant decrease in suspected adverse drug reactions were notes because of de-escalation and discontinuation of few antibiotics.
In terms of HIV, the medical team agreed to shift the patient from general medical ward to HIV special consultancy ward, so further investigation was done under newly charged post graduate trainees.
Our main motive was reducing the cruciality of antibiotic use in HIV to reduce potential multidrug resistance.
Discussion
Antimicrobial stewardship is an efficient model for antibiotic management in severe infections. It includes a rationale formula of assessment with the 5D’s formula:5
- Right Drug
- Right Dose
- Right Dosage Form
- Right Diagnosis
- Right Duration
With infections like HIV, provider mostly prescribe broad spectrum antibiotics. With robust decision-making in emergency department (ED) environments, there is an opportunity for infectious disease pharmacists to provide medication reviews, which can reduce the chances of potential medication errors in certain cases. Pharmacists are trained in managing concurrent therapies and to understand the nuances of dose adjustments, dose calculations, and antibiotic selection.
This case study demonstrates the significance of antimicrobial stewardship in the hospital setting, especially those presenting in the ED, for the management of patients with chronic infectious disease and acute infections. It also explains the criticality of correct therapy management for patients struggling with undiagnosed HIV or those not adequately managed.
The role of infectious disease pharmacists in improving and conducting such stewardship programs is highly encouraging because this activity enhances patient outcomes which gives confidence to the overall medical team.
References
1. Pougnet R, Pougnet L. Principaux rappels à propos de l’histoire du sida et du VIH [A little background on the history of AIDS and HIV]. Rev Infirm. 2022;71(286):16-18. doi:10.1016/j.revinf.2022.12.003
2.Silva B. The Origins of HIV and the AIDS Pandemic. Pages 210–216. March 2022 DOI: 10.1093/oso/9780192863843.003.0027
3.Klinger T. (2023). Hiv. 89-C9N28. doi:10.1093/oso/9780197626528.003.0009
4. World Health Organization. (2023). Antimicrobial resistance: Global report on surveillance 2023. Geneva, Switzerland: World Health Organization.
5. Infectious Diseases Society of America (IDSA) & Society for Healthcare Epidemiology of America (SHEA). (2016). Appropriate Antibiotic Use for Adults: Diagnosis, Selection, and Dosing.Clinical Infectious Diseases, 63(10), e106-e152. https://doi.org/10.1093/cid/ciw331