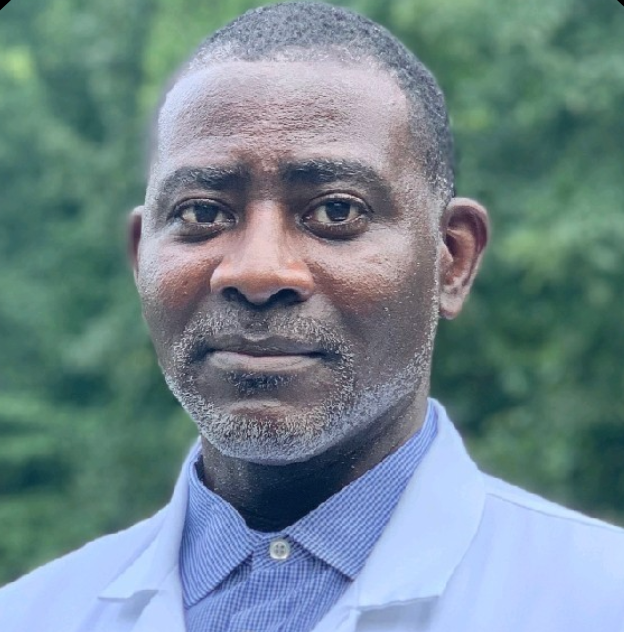
Anson K. Wurapa, MD
Image credits: LinkedIn

At IDWeek, Anson K. Wurapa, MD, presented on the efficacy and safety of bictegravir/emtricitabine/tenofovir alafenamide (B/F/TAF) over five years in Black people with HIV (PWH). By year five, B/F/TAF maintained high rates of virologic suppression in Black PWH, even though a greater proportion had low adherence compared to their non-Black counterparts. Additionally, B/F/TAF was well tolerated, with fewer Black PWH experiencing treatment-emergent adverse events (TEAEs). These findings support the long-term use of B/F/TAF in Black PWH.
In an exclusive interview with Wurapa, an infectious disease specialist at the Infectious Disease Specialists of Atlanta, we discussed the study’s implications for treatment-naive Black adults and compared the results to other populations. Wurapa highlighted the overall high adherence and biological suppression observed in both Black and non-Black patients. He noted that Black patients exhibited slightly lower adherence due to social and economic factors, “Things like social economics, access to care in general. As we know, there’s always been issues in the Black community with health access, issues with mental health, substance abuse, etc, that all impact patients’ ability to adhere to their medications,” Wurapa said.
In total, 211 Black and 421 non-Black PWH received B/F/TAF up to Week 240. At this point, 97.2% of Black PWH and 99.3% of non-Black PWH had HIV-1 RNA levels below 50 copies/mL. Adherence rates revealed that 11.2% of Black PWH had low adherence (less than 85%), compared to 5% of non-Black PWH. Additionally, 20.4% of Black PWH experienced TEAEs related to the study drug, while 31.8% of non-Black PWH reported similar issues. Baseline data showed that rates of hypertension and diabetes were similar in both groups.
“And specifically looking at things like biologic suppression, both groups had high adherence,” Wurapa noted. “The medication was well tolerated. Very few people discontinued the medications, and a very small proportion of Black patients had any treatment-related adverse events.”
Wurapa further discussed how this study addressed the unique health challenges faced by Black adults in treatment. He emphasized the importance of encouraging adherence, stating, “Issues of adherence within the study included pill counts that are part of these analyses, and there’s always an effort within the study to try to encourage adherence. That’s not unique to this study; things are done to try to improve adherence within the studies, and this study was no different in that regard.”
This analysis pooled data from two Phase 3 randomized, double-blind studies (1489 and 1490) comparing B/F/TAF with other regimens in adult PWH. It includes outcomes from Black and non-Black participants during a 144-week randomization phase and a 96-week open-label extension, examining demographics, virologic outcomes, adherence, TEAEs, and changes in CD4 counts and metabolic parameters.
Wurapa concluded by discussing the implications of these studies for future HIV treatment protocols aimed at improving health outcomes in Black communities. “From the patient standpoint, I think it improves their confidence and trust in what they’re being asked to take, knowing that it has actually been looked at in their specific demographic. It does go a long way towards trying to dispel some of those issues when you’re able to talk to them about the fact that.”
He also highlighted the clinician’s perspective, “When you’re sitting with a patient in front of you and having to make decisions about their care and treatment options, it’s always nice to have data that you can present to them as part of your discussion. It also helps the clinician feel comfortable with medication that has been studied specifically in the demographic that’s sitting in front of them.”
To conclude, Black communities are disproportionately affected by HIV and may face greater lifetime risks of comorbidities compared to non-Black PWH. Historically, they have been underrepresented in clinical studies, which can impact the effectiveness of treatment strategies. Wurapa noted, “We found that even taking that into account during treatment, there was no increase in patients developing those conditions while on treatment compared to non-Black patients.” These findings underscore the importance of inclusive research in developing effective treatment protocols and improving health outcomes in Black communities, paving the way for future studies to address healthcare disparities and enhance patient care.







uvk0sw