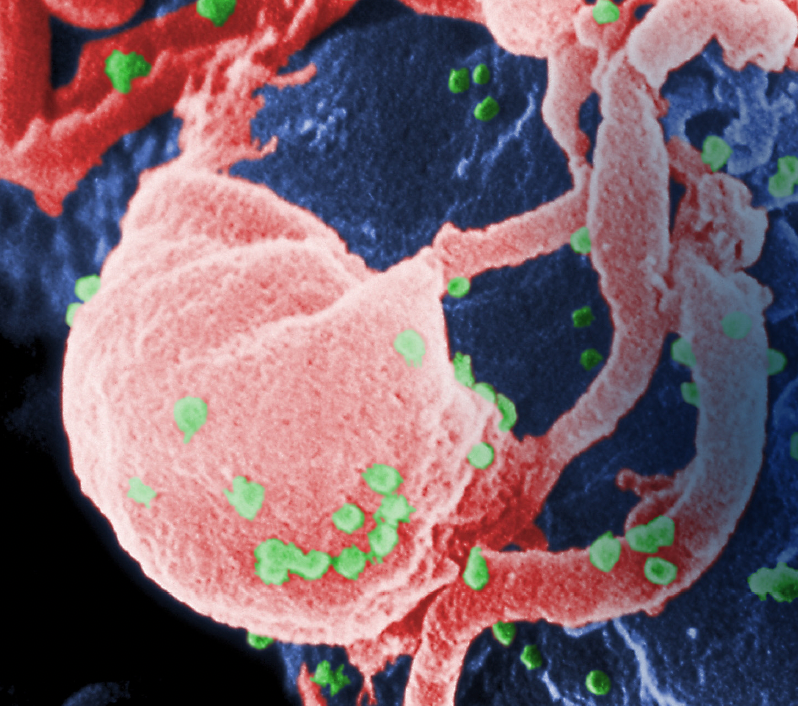
Image credit: C. Goldsmith; Content Providers: CDC/ C. Goldsmith, P. Feorino, E. L. Palmer, W. R. McManus

HIV is a single-stranded RNA virus that can be transmitted through sexual intercourse, during pregnancy from mother to child, as a result of hypodermic needle use, or through infected blood transfusions.1,2 The World Health Organization (WHO) estimates there were 39.9 million persons living with HIV (PLWH) at the end of 2023.3 The incidence of HIV and HIV-associated mortality has decreased by 39% and 51%, respectively, since 2010.3 This progress is partly due to the development of antiretroviral (ARV) medication that allows for HIV RNA suppression (undetectable HIV levels). Combination ARVs, or antiretroviral therapy (ART), have been shown to significantly improve survival, reduce HIV RNA levels, and reduce ART resistance to HIV in PLWH.2,4,5 While receiving ART, a phenomenon can occur where patients can present with a low level of virus that is detectable but still clinically suppressed, known as low-level viremia (LLV).6,7 Currently, there is minimal guidance from contemporary HIV guidelines from the US Department of Health and Human Services (DHHS), the European AIDS Clinical Society (EACS), and the WHO on how to manage LLV. The purpose of this article is to review the clinical significance of patients with LLV and the current literature surrounding the management of LLV in PLWH.
Clinical guidelines developed by the DHHS, EACS, and WHO all define clinical success differently. The WHO defines clinical success as an HIV RNA level of 1000 copies/mL or lower, whereas 200 copies/mL or lower and 50 copies/mL or lower are used by the DHHS and EACS, respectively, at which points HIV transmission and complications are low.8-10 Even while receiving effective therapy, PLWH can develop LLV. The incidence of LLV ranges from 18% to 34% per the DHHS (HIV RNA levels, < 200 copies/mL) and WHO definitions (HIV RNA levels, 50-1000 copies/mL) shown in the TABLE.7-9 Subcategories of LLV have been defined in literature as follows: very LLV (VLLV), fewer than 50 copies/mL; LLV, 50 to 200 copies/mL; and high LLV (HLLV), 200 to 999 copies/mL.7,11,12 This article will use the definitions of VLLV, LLV, and HLLV to better describe the viral level cutoffs reported in the current literature.
Though clinically suppressed, patients with low levels of HIV are not living without risk, especially if the LLV persists, also known as persistent LLV (PLLV). PLLV and HLLV (PHLLV) have been associated with a higher risk of developing severe non-AIDS-associated conditions such as cancers, cardiac-related events, vascular disease, liver cirrhosis, and chronic kidney disease.11 Persistent VLLV (PVLLV), PLLV, and PHLLV have been associated with chronic immunological activation and inflammation.6,13-15 As a result, data from studies have shown weakened cytotoxic T-cell activity concerning reduced HIV clearance and increased cardiac inflammatory markers associated with a risk of developing cardiovascular disease.6,13-15 Virologic failure (VF), virological nonsuppression (at least 2 HIV RNA levels at ≥ 1000 copies/mL), and resist-ance to first-line ART were also associated with PVLLV, PLLV, and PHLLV.6,7,16-21
Of note, the DHHS, EACS, and WHO discuss VF differently, and the ranges of more than 200 copies/mL to more than 1000 copies/mL are all represented in the literature presented here for VF (TABLE). The risk of transmission has not been well studied for PLWH who have PLLV, but patients enrolled in the PARTNER studies (PARTNER1 and PARTNER2) with viral loads of fewer than 200 copies/mL were or lower and 50 copies/mL or lower are used by the DHHS and EACS, respectively, at which points HIV transmission and complications are low.8-10 Even while receiving effective therapy, PLWH can develop LLV. The incidence of LLV ranges from 18% to 34% per the DHHS (HIV RNA levels, < 200 copies/mL) and WHO definitions (HIV RNA levels, 50-1000 copies/mL) shown in the TABLE.7-9

Subcategories of LLV have been defined in literature as follows: very LLV (VLLV), fewer than 50 copies/mL; LLV, 50 to 200 copies/mL; and high LLV (HLLV), 200 to 999 copies/mL.7,11,12 This article will use the definitions of VLLV, LLV, and HLLV to better describe the viral level cutoffs reported in the current literature.
Though clinically suppressed, patients with low levels of HIV are not living without risk, especially if the LLV persists, also known as persistent LLV (PLLV). PLLV and HLLV (PHLLV) have been associated with a higher risk of developing severe non-AIDS-associated conditions such as cancers, cardiac-related events, vascular disease, liver cirrhosis, and chronic kidney disease.11 Persistent VLLV (PVLLV), PLLV, and PHLLV have been associated with chronic immunological activation and inflammation.6,13-15 As a result, data from studies have shown weakened cytotoxic T-cell activity concerning reduced HIV clearance and increased cardiac inflammatory markers associated with a risk of developing cardiovascular disease.6,13-15 Virologic failure (VF), virological nonsuppression (at least 2 HIV RNA levels at ≥ 1000 copies/mL), and resist-ance to first-line ART were also associated with PVLLV, PLLV, and PHLLV.6,7,16-21 Of note, the DHHS, EACS, and WHO discuss VF differently, and the ranges of more than 200 copies/mL to more than 1000 copies/mL are all represented in the literature presented here for VF (TABLE).
The risk of transmission has not been well studied for PLWH who have PLLV, but patients enrolled in the PARTNER studies (PARTNER1 and PARTNER2) with viral loads of fewer than 200 copies/mL were changes.9 Based on DRT results, patients can be switched to a susceptible drug class or add a drug class with a novel mechanism of action (eg, lenacapavir, maraviroc).9 It is also suggested that the new ART include at least 1 drug with a high barrier to resistance (eg, bictegravir, dolutegravir, boosted darunavir).9 The resistant ART should be discontinued, and HIV RNA should be monitored every 4 to 8 weeks.9 This current guidance is concerning for patients with PVLLV and PLLV, especially because these 2 groups are associated with the development of VF and ART resistance. Primary literature guidance for the management of PLLV and PVLLV is scarce. Like the DHHS recommendation for PHLLV, it may be beneficial to use DRT to guide therapy in patients with PLLV. Data from a retrospective cohort study of 1607 patients found 21 patients who had PLLV.28 Of these 21 patients, 8 were receiving unoptimized therapy (on ART with known resistance or on low-potency ART).28
When their ART was optimized or intensified, 6 of the 8 patients achieved virologic suppression (undetectable virus).28 Another retrospective cohort study of 304 PLWH with PLLV assessed DNA-based DRT-guided ART switches.29 VF ( failure to obtain a viral load < 20 copies/mL at 6 months post switch) was lower in those with a guided switch than in those who remained on therapy (5% vs 19%; P = .02).29 Maintenance of virologic suppression was significantly higher after DRT-guided ART switch than in those who continued on therapy 6 months after DRT was performed (P = .0006).29
Of these switches, the primary methods were a switch to an INSTI-based regimen, a single-tablet regimen, or de-escalation to second-line therapy.29 In a review of 7 studies including PLWH with PLLV, data revealed that modifying or intensifying ART resulted in decreased incidences of VF.30 No studies have discussed using DRT as guidance for ART management in patients with PVLLV. Considering the paucity of data and relatively high incidence (18%-34%) for patients with persistently low levels of virus over their course of treatment, more research and guidance are needed to help determine appropriate management. Guideline revision is essential, especially for the DHHS guidelines, which state that patients with an HIV RNA level fewer than 200 copies/ mL do not require ART modification, as PLLV and PVLLV have been associated with VF, virologic non-suppression, and ART resistance. The development of non-AIDS-defining events has been associated with PLLV, leading to poor clinical outcomes. Current literature and guidelines suggest using DRT to guide therapy in these cases, yet DRT may not always be available and could be cost-prohibitive, especially in low-and middle-income countries.31 Another limitation of DRT is that the FDA approved DRT assays require levels of at least 1000 copies/mL (TRUGENE HIV-1 Genotyping Kit), which by definition would prevent testing for resistance in patients with PVLLV, PLLV, or PHLLV.32 Evidence from 1 study demonstrated successful genotyping at viral levels as low as 100 copies/mL with these switches, the primary methods were a switch to an INSTI-based regimen, a single-tablet regimen, or de-escalation to second-line therapy.29
In a review of 7 studies including PLWH with PLLV, data revealed that modifying or intensifying ART resulted in decreased incidences of VF.30 No studies have discussed using DRT as guidance for ART management in patients with PVLLV. Considering the paucity of data and relatively high incidence (18%-34%) for patients with persistently low levels of virus over their course of treatment, more research and guidance are needed to help determine appropriate management. Guideline revision is essential, especially for the DHHS guidelines, which state that patients with an HIV RNA level fewer than 200 copies/ mL do not require ART modification, as PLLV and PVLLV have been associated with VF, virologic non-suppression, and ART resistance. The development of non-AIDS-defining events has been associated with PLLV, leading to poor clinical outcomes. Current literature and guidelines suggest using DRT to guide therapy in these cases, yet DRT may not always be available and could be cost-prohibitive, especially in low-and middle-income countries.31
Another limitation of DRT is that the FDA approved DRT assays require levels of at least 1000 copies/mL (TRUGENE HIV-1 Genotyping Kit), which by definition would prevent testing for resistance in patients with PVLLV, PLLV, or PHLLV.32 Evidence from 1 study demonstrated successful genotyping at viral levels as low as 100 copies/mL with detectable virus.33 Still, DRT may not detect all resistances, especially archived viruses, or viruses with resistance stored away in the HIV reservoir.9 These resistances can reemerge under selective drug pressure even if absent from initial or subsequent DRT results.9 The DHHS suggests an HIV-1 proviral DNA resistance assay to detect resistance of archived virus below the limit of detection in standard DRT or in patients with low-level viremia, though this method can still miss resistance at levels of DNA <83 copies/mL.9








330nrs