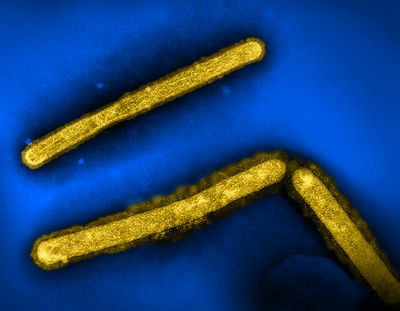
Three influenza A (H5N1/bird flu) virus particles (rod-shaped; yellow). Note: Layout incorporates two CDC transmission electron micrographs that have been repositioned and colorized by NIAID.
Image credit: CDC and NIAID

The National Institutes of Health (NIH) updated its risk assessment for highly pathogenic H5N1 avian influenza A virus (HPAI H5N1) saying the risk to the general public remains low.
The NIH’s National Institute of Allergy and Infectious Diseases (NIAID) leadership including NIAID Director Jeanne M. Marrazzo, MD, MPH, and Michael G. Ison, MD, MS, chief of the Respiratory Diseases Branch in NIAID’s Division of Microbiology and Infectious Diseases said in a new commentary published in the New England Journal of Medicine, that people should find a balance between enhanced vigilance and “business as usual” with respect to avian influenza.
In the commentary, they discuss 4 strategies how we can respond to the threat including:
1.“collaboration among investigators in human and veterinary medicine, public health leadership, health care providers, and occupational authorities,
2. the urgent need for vigilant surveillance of emerging mutations and assessment of the threat of human-to-human transmission,
3. pursue development and testing of medical countermeasures, and
4.precautions to prevent infection are critical, including the use and optimization of PPE in occupational settings and education about the risk of contact with sick birds and animals.” 1 (See below for some infection prevention strategies from Marrazzo.)
Thus far, the overwhelming majority of cases have been in farm workers who are working with cattle and poultry. All cases in the United States, except 1 have been classified as mild. The single case of severe avian influenza has been reported in a 65-year old person who had a different genotype of the virus, D11.2
In the Journal commentary, Marrazzo and Ison point out a case in Canada of a young girl who also had the D11 genotype and was hospitalized with a very severe case including having to be put on venovenous extracorporeal membrane oxygenation (ECMO). She had existing mild asthma and obesity and presented with conjunctivitis and fever and had progression to respiratory failure. After ECMO and treatment with antivirals, she recovered.1
As of today, January 3, 2025, there have been 66 cases of avian influenza in the US according to the CDC’s website. And the agency points at there have only been zoonotic transmissions in humans and no human to human transmission. 3
Contagion interviewed Marrazzo recently who offered infection control prevention strategies for both farm workers and the general public.
What You Need to Know
The NIH and CDC emphasize that the risk of H5N1 avian influenza to the general public remains low.
While most US cases have been mild, severe instances like the single severe U.S. case and in Canada underscore the potential danger posed by genetic mutations of the virus (eg, D11 genotype).
NIH continues to stress the need to focus on prevention and response strategies.
“The CDC recommends avoiding direct contact with wild birds or other wild animals, especially if they appear to be sick or dead. Wild birds can also be infected with H5N1 and not appear sick, so it is better to observe them from a distance. People who live and work alongside domesticated animals which may be potentially infected, such as poultry or dairy cattle, can take extra precautions to avoid contact with infected animals and their contaminated environments. For example, wearing personal protective equipment can help dairy farm workers reduce exposure to infectious milk,” Marrazzo said.
“While there are no documented cases of humans directly catching H5N1 influenza from drinking raw unpasteurized milk, raw milk produced by cattle infected with H5N1 contains high levels of the virus. Fortunately, pasteurization appears to kill the flu virus. Because of the risk of exposure to the H5N1 flu virus, as well as other harmful diseases, people should not consume raw milk or products, such as fresh cheese, that are made with raw milk.”
In their commentary, Marrazo and Ison succinctly offer their assessment of where we are today at the beginning of 2025 as it regards this strain of influenza.
“The CDC still designates the risk of HPAI A(H5N1) to most Americans as low. We do have candidate vaccines and antivirals available to try to mitigate severe influenza in the case of wider spread… The past weeks have seen more cases detected in more states as well as more persons with respiratory illness acquired through exposure to poultry or from an unknown source. Without a clearer understanding of the extent of exposure, infection, viral evolution, and transmission, we will be unable to properly protect our communities from a pathogen that has proven to be a formidable challenge to human and animal health,” they write.1