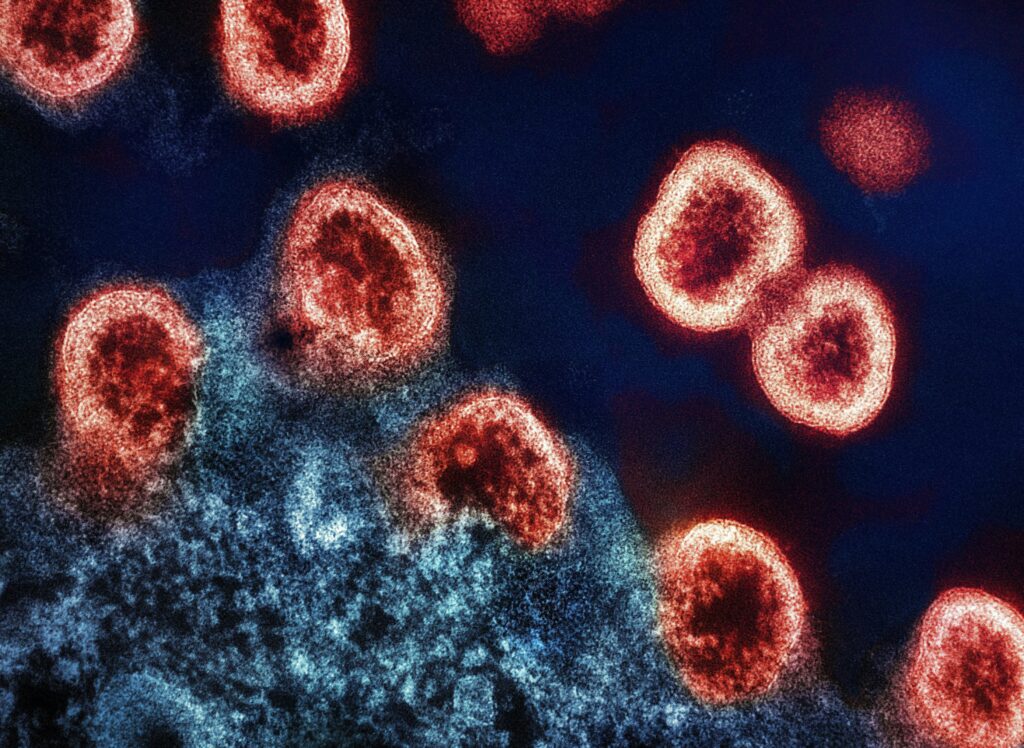
HIV-1 Virus Particles Transmission electron micrograph of HIV-1 virus particles (colorized red) replicating from an HIV-infected H9 T-cell (blue).
Image credit: NIDID

In the last few years, Gilead’s lenacapavir (Sunlenca) has seen a lot of movement that include a CRL, FDA approval, potentially a new indication looking at HIV prevention, and even a call for it to become an HIV vaccine. Recent data coming from a trial in South Africa demonstrated its possible utility as an HIV prevention tool. And to add more intrigue to lenacapavir, during this week’s International AIDS Society 2024 conference, there has been a call to consider it as a potential HIV vaccine.
Multidrug Resistant Therapy
Lenacapavir was initially developed as therapy for adult patients living with HIV, whose infections could not be successfully treated with other available treatments due to resistance, intolerance, or safety considerations. Multidrug resistance is an ongoing clinical management challenge, and in this space, there is limited options.
In March of 2022, Gilead received a complete response letter (CRL) from the FDA. The letter cited Chemistry Manufacturing and Controls (CMC) issues relating to the compatibility of lenacapavir with the proposed container vial as the reason for their action.
The CRL was not reflective of the therapy itself.
“Gilead intends to provide FDA with a comprehensive plan and corresponding data to use a different vial type. We look forward to discussing this further with FDA over the coming months so that we can make this investigational new therapy available to people living with multidrug-resistant HIV as soon as possible,” Gilead Chief Medical Officer Merdad Parsey, MD, PhD, said in a statement at the time.1
Gilead worked with the FDA to provide the federal agency with the information and compliance that was needed, and when it was FDA approved in December 2022, it was a welcome addition for patients and clinicians.
“Today’s approval ushers in a new class of antiretroviral drugs that may help patients with HIV who have run out of treatment options,” Debra Birnkrant, MD, director of the Division of Antivirals in the FDA’s Center for Drug Evaluation and Research, said in a statement when it was approved.1
Lenacapavir is the first of a new class of therapies called capsid inhibitors to be FDA-approved for treating HIV. This antiretroviral works by blocking the HIV-1 virus’ protein shell (the capsid), thereby interfering with multiple essential steps of the viral lifecycle. The approval was based from the data of the CAPELLA study, which was a double-blinded, placebo-controlled global multicenter trial designed to evaluate lenacapavir when administered every 6 months as a subcutaneous injection in heavily treatment-experienced (HTE) people with multi-drug resistant (MDR) HIV infection.1
Overall, 72 participants were enrolled with 36 in each of the 2 cohorts. In terms of the makeup of the participants, 25% were female, 38% Black, the median age 52 years, 19% had VL > 100k c/mL, 64% had CD4 <200 cells/μL, 46% had HIV-1 resistant to all 4 major classes (NRTI, NNRTI, PI, INSTI), and 17% did not have any fully active agents in the optimized background regimen (OBR).1
In cohort 1 (randomized group), participants were assigned (2:1) to add oral lenacapavir or placebo to their failing regimen (600 mg on Day 1[D] and 2 and 300 mg on D8). At Day 15, those on oral lenacapavir received subcutaneous (SC) lenacapavir 927 mg every 6 months; those on placebo started the 2 week oral lead-in, followed by SC Q6M. All randomized participants initiated an investigator-selected, OBR at D15 the investigators explained.1
In cohort 2 (non-randomized group), the participants started OBR concurrent with lenacapavir (oral lead-in → SC). The investigators reported the secondary endpoint of W52 efficacy by FDA-snapshot algorithm in the randomized cohort and additional available efficacy and safety from both cohorts.1
Earlier this year, new data was presented at the CROI meeting that demonstrated treatment benefits over a 2-year period from the phase 2/3 CAPELLA trial evaluating the lenacapavir.2
“We found even as far out as two years or the so called 104 [week] data, that about 82% of individuals—when we excluded those who are missing— were virologically suppressed…that’s unheard of numbers for this kind of patient population,” Onyema Ogbuagu, MBBCh, FACP, FIDSA, director of HIV Clinical Trials program at Yale School of Medicine, and principal investigator on the trial said in an earlier interview with Contagion. “We have other studies with other agents that have shown lower rates of treatment success with these kinds of patients.”2
Read more: Examining a Newer Therapy for Heavily Treated HIV Patients
HIV Prevention
One of the bigger developments around the antiviral has been the recent data related to lenacapavir as a potential HIV prevention tool.
Last month, the company announced significant findings from its phase 3 PURPOSE 1 trial, that showed a 100% efficacy in preventing HIV infection among cisgender women. The trial included more than 5300 participants from both South Africa and Uganda.3
The second phase of the study will span from 1 to 3 years, with participant visits occurring every 4-13 weeks, totaling between 4 and 8 visits annually. Each participant in this phase will receive both a daily pill and a semiannual injection, with one containing the active drug and the other serving as a placebo.3
Read more: Lenacapavir’s 100% Efficacy: Gilead’s Step Towards HIV Prevention
A Possible Vaccine?
At the ongoing IAS HIV conference, a poster presented by Fortunak et al and coinvestigators offered some analysis looking at utilizing lenacapavir as a vaccine. Specifically, they wrote it could be mass-produced under a voluntary license for approximately $40 per person year at scale. They said lenacapavir is currently charging $40,000 per person-year for it in high-income countries.4
They put forth 2 hypothesis: could the lenacapavir injectable be priced at $100 person-year at a committed demand of 1 million people per year; or could the Cost of Goods (COS) eventually be competitive with oral PrEP?4
Lenacapavir has both oral and injectable modalities currently in usage.
It remains to be seen how Gilead views these hypotheses; however, from today’s press statement, it appears the company is planning to move forward with a strategy to utilize lenacapavir as PrEP. “Gilead is building an access strategy that prioritizes speed and enables the most efficient path for the regulatory approval of twice-yearly lenacapavir for PrEP in countries that account for most of the global disease burden.”5
References
1.Sunlenca (lenacapavir) Receives FDA Approval as a First-in-Class, Twice-Yearly Treatment Option for People Living With Multi-Drug Resistant HIV. Gilead news statement. December 22, 2022. Accessed July 24, 2024.
https://www.contagionlive.com/view/fda-approves-lenacapavir-for-hiv-treatment